Morgan Birch never imagined her four-month-old daughter, Kimie, would catch measles. The Alberta mother initially thought Kimie's fever and rash were from routine vaccinations or chicken pox. But her grandmother quickly identified the illness: "That's measles." Lab tests confirmed the diagnosis, and Kimie became part of a troubling statistic—over 3,800 measles cases in Canada so far in 2025, largely involving children and infants.
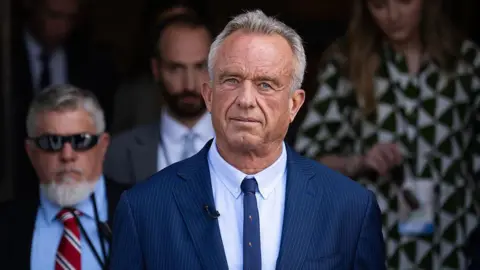
This alarming figure stands out, as it is nearly three times the case count in the US, despite Canada's smaller population. According to CDC data, Canada ranks eighth worldwide for measles outbreaks, and Alberta has the highest rate of infection in North America. Questions are being raised about whether Canadian health authorities are doing enough to manage the situation, particularly when vaccine-hesitant figures, like public health advocate Robert F. Kennedy Jr. in the US, are absent in Canada.
The measles epidemic reflects a broader resurgence of the virus in North America, Europe, and the UK. In the US, measles cases have reached a 33-year high, while England reports its highest rates since 2012. Measles was declared eliminated in Canada in 1998, and 2025 marks the highest number of cases since then, surpassing the previous peak of 750 cases in 2011. The MMR (measles, mumps, rubella) vaccine has shown to be 97% effective, yet vaccination rates have declined significantly, especially among select communities.
The outbreak’s origin in Canada can be traced back to a large Mennonite gathering in New Brunswick, where vaccination rates are historically lower due to cultural beliefs. Areas in southwestern Ontario and Alberta have been hit hardest, with Ontario reporting over 200 new cases weekly at the outbreak's peak in April. Dr. Vivien Suttorp, Alberta's medical officer of health, noted that the rapid spread overwhelmed public health efforts to trace the original source.
Catalina Friesen, a healthcare worker aiding the Mennonite community, noted the unprecedented nature of this outbreak. Many infected individuals were unvaccinated, challenged by a growing wave of anti-vaccine misinformation since the Covid-19 pandemic. Distrust in the healthcare system further complicates vaccination efforts within these communities, which have long grappled with perceptions of being ostracized.
Despite these challenges, health officials stress the importance of increasing vaccination rates. Janna Shapiro from the University of Toronto highlights that without a concerted effort to immunize, outbreaks will continue. In southern Alberta, MMR vaccinations plunged nearly 50% from 2019 to 2024. The public's resistance to Covid-19 vaccine mandates has sparked hesitancy toward other vaccines.
With a reduction of the measles vaccination age in Alberta and intensified public outreach campaigns, health units across Canada are working to mitigate the crisis. However, the public's response remains lukewarm compared to mobilization seen during the pandemic, leaving small children like Kimie vulnerable.
Birch is understandably upset by the measles infection and urges parents to prioritize vaccinations. "It's frustrating for those who refuse to vaccinate," she lamented, asserting that her daughter should not have contracted the disease in 2025.